When television personality Christine Brown Woolley opened up about her oxycodone addiction, she helped shine a light on a serious issue many don’t see coming: a short-term prescription turning into something more. In this article, you’ll learn how oxycodone works, why post-surgery prescribing can lead to dependence, and what you can do if you or a loved one faces opioid challenges.
Christine’s Story: From Prescription to Dependence
In her memoir Sister Wife, released on September 2, 2025, Christine Brown Woolley opens up about her private struggle with a brief oxycodone addiction that unfolded offscreen. She explained, “It gave me the best high I ever felt… I was on top of the world.”
After tearing her ACL and meniscus, Christine was prescribed oxycodone. She recalled how, after returning home from surgery, her then-husband Kody handed her a bag of pain pills with little guidance on what to do next. “What do I need to do?” she asked, unsure about her aftercare, but there were no clear instructions, only the filled prescription. That moment marked the quiet beginning of what would become her brief struggle with oxycodone dependency.
What Is Oxycodone and Why Is It Risky?
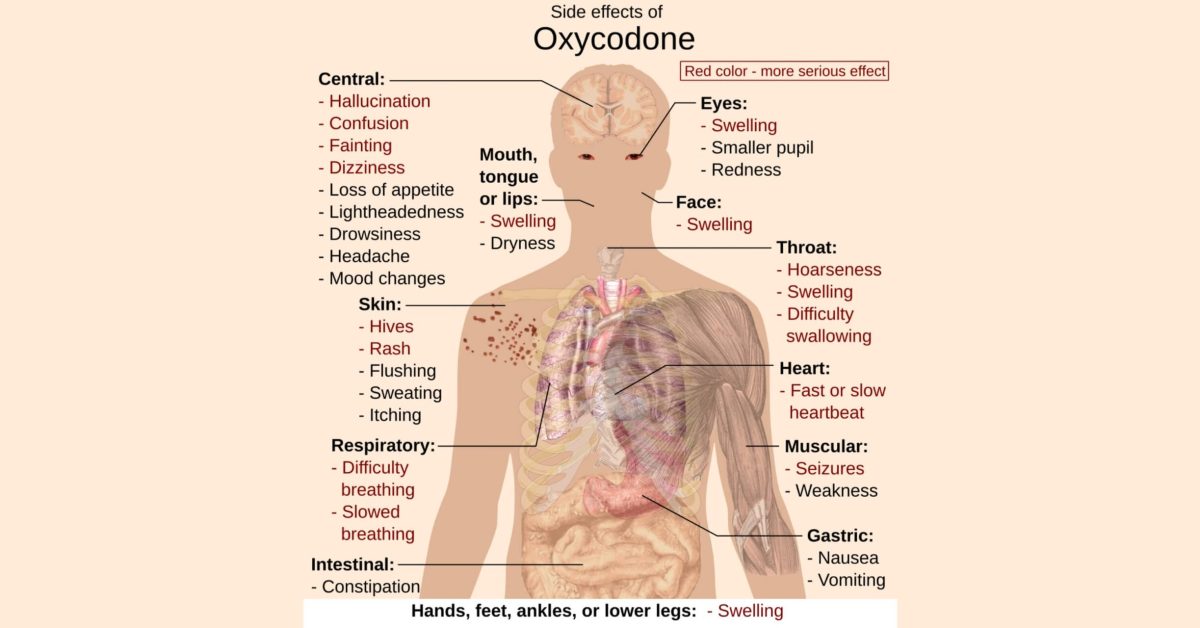
Oxycodone is a powerful opioid pain-reliever often prescribed after surgery or injury. According to the Centers for Disease Control and Prevention (CDC), even short-term use, taken as prescribed, can sometimes lead to dependence if not managed carefully. Because it relieves pain quickly, it can mask both the underlying injury and the early warning signs of misuse.
Key risk factors include:
- Post-surgery pain (e.g., knee or hip repair)
- Prescriptions without clear tapering plans
- History of mental health or substance use issues
- Lack of education on safe storage and disposal
The CDC’s updated opioid-prescribing guideline provides recommendations for clinicians treating acute, subacute, and chronic pain in adults, focusing on when to start opioids, selecting and dosing medications, determining prescription duration with follow-up, and managing risks and potential harms.
What You Can Do: Prevention and Treatment
Opioids can be helpful for pain, but they carry serious risks. Being aware of warning signs, practicing safe use, and knowing treatment options can protect your health and support recovery.
Recognizing the Warning Signs
- Taking pain pills when you’re no longer in significant pain
- Feeling like you “need” the pill to function or feel normal.
- Hiding or minimizing your use
Safe Prescribing & Tapering
- Ask your provider how long you’ll need opioids, and request a tapering schedule.
- Store prescribed opioids securely and dispose of any unused medication (see U.S. FDA’s guidelines).
- Consider non-opioid alternatives such as NSAIDs, physical therapy, or other treatments.
Treatment Options for Opioid Use
- Detoxification: Safely manages withdrawal symptoms at the start of treatment
- Medication-assisted treatment (MAT): Vivitrol, buprenorphine, and methadone can help reduce cravings and prevent relapse.
- Behavioral therapy & support: Counseling, therapy, and sober-living programs offered through inpatient or outpatient treatment help strengthen long-term recovery.
Ready to Begin Your Own Recovery Journey?
At Sunrise Recovery in Clarksville, Jeffersonville, and Lafayette, Indiana, we believe that early intervention can make all the difference. If you or a loved one is navigating potential opioid dependence or addiction, you don’t have to go it alone.
Contact us today to verify insurance and start a tailored inpatient or outpatient program that fits your needs.
Each type of stigma compounds the others, creating emotional, social, and structural barriers to health and recovery.
FAQs on Opioids & Oxycodone Addiction
Signs include taking pain pills when pain is minimal, feeling like you need the medication to function, or hiding your use. Christine Brown’s story shows how quickly short-term prescriptions can lead to dependency.
Yes. Even brief prescriptions can cause dependence, especially without proper tapering or monitoring. Pain relief can mask early warning signs of misuse.
MAT uses FDA-approved medications like Vivitrol, buprenorphine, or methadone alongside counseling. It reduces cravings, prevents relapse, and supports long-term recovery.
Follow your provider’s tapering plan, store pills securely, and dispose of unused medication according to FDA guidelines. Safe handling reduces risk for misuse or accidental overdose.
Treatment can include detoxification to manage withdrawal, MAT to reduce cravings, and behavioral therapy with counseling or sober-living programs. Both inpatient and outpatient programs are effective depending on individual needs.
Listen without judgment, encourage professional help, and assist with practical tasks like appointments or safe medication disposal. Supportive involvement improves recovery outcomes.
If you or someone you care about is struggling with addiction, please contact the SAMHSA Helpline at 1-800-662-HELP (4357).